Patient education
Here are the answers to some frequently asked questions:
Pap Smear
WHAT IS A PAP SMEAR?
A pap smear is a test that is done on the cervix, located in the upper vagina. The cervix is the opening to, or bottom portion, of your uterus. A Pap Smear is a test that checks for abnormal cells and serves as an important screening tool for early signs of cervical cancer. A Pap Smear is also sometimes referred to as a Pap test or Papanicolaou test. The procedure involves your doctor taking a small sample of cells from your cervix and sending them to a laboratory to be read.
WHY GET A PAP SMEAR?
Regular screening is important and is part of a preventive healthcare plan. Your doctor will recommend how often you should have a Pap Smear. Research and clinical guidelines show that almost all cervical changes can be found with regular screening and treated before they become cancerous.
HOW OFTEN SHOULD I GET A PAP SMEAR?
Women should talk with their doctor about when to start screening and how often to be screened. In 2018, the United States Preventive Services Task Force updated the screening guidelines. These are guidelines, your doctor will recommend how often you should be screened based on your history, health status, family history, and risk factors.
HOW SHOULD I PREPARE FOR A PAP SMEAR?
To make sure your test is as accurate as possible these simple recommendations are often advised. Always verify specific pre-procedure instructions with your healthcare provider.
WHO CAN PERFORM MY PAP SMEAR?
Your Doctor, a Physician Assistant, or a Nurse Practitioner will perform your Pap Smear. If your practitioner is a male, you can ask for a chaperon to be present in the room. At Hermes Health all providers are female.
A pap smear is a test that is done on the cervix, located in the upper vagina. The cervix is the opening to, or bottom portion, of your uterus. A Pap Smear is a test that checks for abnormal cells and serves as an important screening tool for early signs of cervical cancer. A Pap Smear is also sometimes referred to as a Pap test or Papanicolaou test. The procedure involves your doctor taking a small sample of cells from your cervix and sending them to a laboratory to be read.
WHY GET A PAP SMEAR?
Regular screening is important and is part of a preventive healthcare plan. Your doctor will recommend how often you should have a Pap Smear. Research and clinical guidelines show that almost all cervical changes can be found with regular screening and treated before they become cancerous.
HOW OFTEN SHOULD I GET A PAP SMEAR?
Women should talk with their doctor about when to start screening and how often to be screened. In 2018, the United States Preventive Services Task Force updated the screening guidelines. These are guidelines, your doctor will recommend how often you should be screened based on your history, health status, family history, and risk factors.
- Women ages 21 through 29 should be screened every three years.
- Women ages 30 through 65 should be screened every three to five years.
- Women with certain risk factors may need to have more frequent screenings or be advised to continue screening beyond age 65.
HOW SHOULD I PREPARE FOR A PAP SMEAR?
To make sure your test is as accurate as possible these simple recommendations are often advised. Always verify specific pre-procedure instructions with your healthcare provider.
- Avoid sexual intercourse for two days before your test.
- To avoid washing away or affecting your cervical cells, do not use the following for two to three days before your Pap Smear:
- Tampons
- Birth control foams or gels
- Vaginal medicines, such as those used to treat a yeast infection
- Douches
- Vaginal creams or powders
WHO CAN PERFORM MY PAP SMEAR?
Your Doctor, a Physician Assistant, or a Nurse Practitioner will perform your Pap Smear. If your practitioner is a male, you can ask for a chaperon to be present in the room. At Hermes Health all providers are female.
HOW IS A PAP SMEAR PERFORMED?
Before the procedure, your doctor will obtain a thorough history of your medical status and overall health. Most of these questions will be directed towards your gynecologic history and a review of your general health.
DOES A PAP SMEAR HURT?
The test may be uncomfortable, but it is not usually painful. You may experience less discomfort if you empty your bladder before the procedure. Also, try deep breathing and relaxation techniques during the procedure to relax you and your muscles. Tensing up is neither you nor your doctor’s friend.
WHAT WILL THE RESULTS REVEAL?
Abnormal cells can be cancerous, but they can also be treatable cell changes, rather than cervical cancer.
Some of the cells collected from the cervix during a Pap Smear may also be tested for human papillomavirus (HPV). Infection with HPV is a risk factor for cervical cancer. HPV is commonly passed from person to person during sexual activity. There are different types, or strains, of HPV. Some strains are more strongly linked with certain types of cancer. Your health care provider may test for HPV at the same time as a Pap test. Or you may need testing for HPV only after Pap test results show abnormal changes to the cervix. HPV testing may also be done separately from a Pap test. A Pap Smear along with a pelvic exam may also help find other conditions, such as infections or inflammation.
IS THERE ANYTHING I SHOULD DO AFTER MY PAP SMEAR?
You can resume your normal activities right after having your Pap Smear. It is possible to experience a small amount of vaginal bleeding or spotting after your Pap Smear. Notify your doctor if you have excessive bleeding or cramping.
DISCLAIMER
This patient education page is for information purposes and is not considered individual patient advice. Because of the changing nature of clinical information and recommendations, please always consult and verify with your physician, pharmacist, or health care provider about specific use or questions. Hermes Health represents that the information provided was formulated with a reasonable standard of care, in conformity with professional standards in the field, and researched with reliable and verified sources.
Before the procedure, your doctor will obtain a thorough history of your medical status and overall health. Most of these questions will be directed towards your gynecologic history and a review of your general health.
- Are you pregnant, or could you be pregnant?
- Do you use birth control? What kind?
- What medications are you taking?
- When was your last menstrual period?
- How long did it last?
- What is your normal cycle length?
- Do you have painful periods?
- How heavy is your normal flow? On average, how many pads or tampons per day?
- Have you ever had abnormal results from a previous Pap Smear?
- Do you have any symptoms, such as itching, burning, redness, pain, or sores?
- Have you had surgery or other procedures on your reproductive organs?
DOES A PAP SMEAR HURT?
The test may be uncomfortable, but it is not usually painful. You may experience less discomfort if you empty your bladder before the procedure. Also, try deep breathing and relaxation techniques during the procedure to relax you and your muscles. Tensing up is neither you nor your doctor’s friend.
WHAT WILL THE RESULTS REVEAL?
Abnormal cells can be cancerous, but they can also be treatable cell changes, rather than cervical cancer.
Some of the cells collected from the cervix during a Pap Smear may also be tested for human papillomavirus (HPV). Infection with HPV is a risk factor for cervical cancer. HPV is commonly passed from person to person during sexual activity. There are different types, or strains, of HPV. Some strains are more strongly linked with certain types of cancer. Your health care provider may test for HPV at the same time as a Pap test. Or you may need testing for HPV only after Pap test results show abnormal changes to the cervix. HPV testing may also be done separately from a Pap test. A Pap Smear along with a pelvic exam may also help find other conditions, such as infections or inflammation.
IS THERE ANYTHING I SHOULD DO AFTER MY PAP SMEAR?
You can resume your normal activities right after having your Pap Smear. It is possible to experience a small amount of vaginal bleeding or spotting after your Pap Smear. Notify your doctor if you have excessive bleeding or cramping.
DISCLAIMER
This patient education page is for information purposes and is not considered individual patient advice. Because of the changing nature of clinical information and recommendations, please always consult and verify with your physician, pharmacist, or health care provider about specific use or questions. Hermes Health represents that the information provided was formulated with a reasonable standard of care, in conformity with professional standards in the field, and researched with reliable and verified sources.
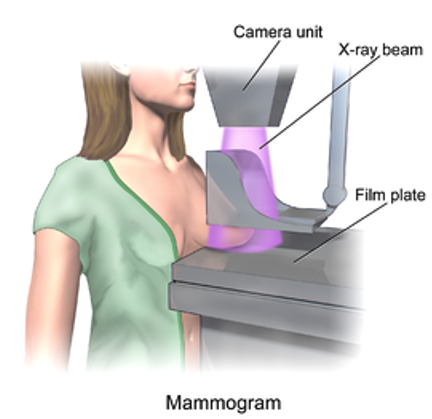
Mammogram
WHAT IS A MAMMOGRAM?
A mammogram is an X-ray of your breasts used to screen for abnormalities in your breast tissue. A screening mammogram is looking for the early signs of breast cancer. There is another type of mammogram, called a diagnostic mammogram, which aids in the diagnosing of lumps, tumors, cysts, or areas of dense breast tissue. The procedure used to obtain these breast X-rays is called mammography. Most modern breast imaging centers use digital technology instead of film. This makes the images much easier to store and share. The images are also sharper and clearer than with film, which can make it easier to see small changes.
WHY GET A MAMMOGRAM?
Your doctor will recommend a screening mammogram as an important part of a preventative healthcare plan. Screenings are looking for early signs of breast cancer. The images will show small tumors or lumps that cannot be felt during a breast examination as well as other breast changes. You may be getting your mammogram as a diagnostic mammogram for your doctor to get a more detailed image of a specific abnormality, or area of concern noted or felt on your yearly breast exam or a previous mammogram.
HOW OFTEN SHOULD I GET A MAMMOGRAM?
The United States Preventive Services Task Force and other agencies and organizations have developed guidelines for mammography screening. Most recommend that women consult with their doctor about the benefits and harms of mammography, when they should start screening, and how often to be screened. This recommendation will be based on your age, family and personal history of cancer, and other risk factors.
HOW SHOULD I PREPARE FOR A MAMMOGRAM?
There is no real preparation before your mammogram. Always check with your doctor or breast care center regarding specific instructions before your mammogram. You can take an over-the-counter pain medication one hour before your appointment if you are concerned about discomfort.
Because you will need to remove your clothing from the waist up and be putting on a front opening hospital gown, you may consider wearing an easy-to-remove top and bra. You will need to remove neck jewelry before the test, so you may want to leave necklaces at home. Depending on your breast care center, the most common recommendations are that you avoid applying the following products the day of your mammogram; deodorant or antiperspirant, body powder, or lotion. These personal care items can leave a residue that may show up on your images.
Let your doctor or mammographer know if you are or could be pregnant.
QUESTIONS YOU MAY WANT TO ASK?
HOW IS THE PROCEDURE PERFORMED?
A mammogram takes about ten to fifteen minutes, but your full appointment can take longer. This would include changing clothes, having the procedure and your mammographer (technician performing the test) making sure the images are clear for the radiologist (a doctor who specializes in reading imaging tests) to read.
During your mammogram, you will stand in front of a special X-ray machine. This machine is tall with two flat plastic plates to compress the breast for imaging. The mammographer will adjust the machine to your height and then rest your breast on the bottom plate. The top plate, the compression plate, will lower onto your breast. You may be asked to take a deep breath before the final compression.
When the breast is flattened between the plates, the machine will take the X-rays from above the breast. This is uncomfortable but does not last long. Your breast needs to be flattened because the X-ray is less powerful than a normal X-ray, and being flattened makes it easier to visualize abnormalities. It also keeps the breast tissue from moving, which would produce a blurry image.
For a preventative screening, you will generally have several images taken of each breast. If you are having a diagnostic mammogram, you may need additional images. The mammographer might have you change positions a few times. After you are done, they will make sure the images are clear. They may retake any pictures that are not clear.
A mammogram is an X-ray of your breasts used to screen for abnormalities in your breast tissue. A screening mammogram is looking for the early signs of breast cancer. There is another type of mammogram, called a diagnostic mammogram, which aids in the diagnosing of lumps, tumors, cysts, or areas of dense breast tissue. The procedure used to obtain these breast X-rays is called mammography. Most modern breast imaging centers use digital technology instead of film. This makes the images much easier to store and share. The images are also sharper and clearer than with film, which can make it easier to see small changes.
WHY GET A MAMMOGRAM?
Your doctor will recommend a screening mammogram as an important part of a preventative healthcare plan. Screenings are looking for early signs of breast cancer. The images will show small tumors or lumps that cannot be felt during a breast examination as well as other breast changes. You may be getting your mammogram as a diagnostic mammogram for your doctor to get a more detailed image of a specific abnormality, or area of concern noted or felt on your yearly breast exam or a previous mammogram.
HOW OFTEN SHOULD I GET A MAMMOGRAM?
The United States Preventive Services Task Force and other agencies and organizations have developed guidelines for mammography screening. Most recommend that women consult with their doctor about the benefits and harms of mammography, when they should start screening, and how often to be screened. This recommendation will be based on your age, family and personal history of cancer, and other risk factors.
HOW SHOULD I PREPARE FOR A MAMMOGRAM?
There is no real preparation before your mammogram. Always check with your doctor or breast care center regarding specific instructions before your mammogram. You can take an over-the-counter pain medication one hour before your appointment if you are concerned about discomfort.
Because you will need to remove your clothing from the waist up and be putting on a front opening hospital gown, you may consider wearing an easy-to-remove top and bra. You will need to remove neck jewelry before the test, so you may want to leave necklaces at home. Depending on your breast care center, the most common recommendations are that you avoid applying the following products the day of your mammogram; deodorant or antiperspirant, body powder, or lotion. These personal care items can leave a residue that may show up on your images.
Let your doctor or mammographer know if you are or could be pregnant.
QUESTIONS YOU MAY WANT TO ASK?
- Where will my mammogram be done?
- Can I request a female mammographer?
- Are there any possible risks of a mammogram?
- How accurate are mammograms at finding breast tissue abnormalities?
- When will I get the results, and how?
- Will my doctor explain the results to me?
- What other tests will I need if the mammogram is not clear or shows signs of cancer?
- Depending on what the image results reveal, you could be referred for
- A diagnostic (follow-up) mammogram
- Breast ultrasound
- Fine needle biopsy
- Referral to a Breast Specialist or Surgeon
- Referral to an Oncologist
- Depending on what the image results reveal, you could be referred for
HOW IS THE PROCEDURE PERFORMED?
A mammogram takes about ten to fifteen minutes, but your full appointment can take longer. This would include changing clothes, having the procedure and your mammographer (technician performing the test) making sure the images are clear for the radiologist (a doctor who specializes in reading imaging tests) to read.
During your mammogram, you will stand in front of a special X-ray machine. This machine is tall with two flat plastic plates to compress the breast for imaging. The mammographer will adjust the machine to your height and then rest your breast on the bottom plate. The top plate, the compression plate, will lower onto your breast. You may be asked to take a deep breath before the final compression.
When the breast is flattened between the plates, the machine will take the X-rays from above the breast. This is uncomfortable but does not last long. Your breast needs to be flattened because the X-ray is less powerful than a normal X-ray, and being flattened makes it easier to visualize abnormalities. It also keeps the breast tissue from moving, which would produce a blurry image.
For a preventative screening, you will generally have several images taken of each breast. If you are having a diagnostic mammogram, you may need additional images. The mammographer might have you change positions a few times. After you are done, they will make sure the images are clear. They may retake any pictures that are not clear.
DOES THE TEST HURT?
The test can be uncomfortable and some women do find it painful. You will experience a feeling of pressure. The level of discomfort or pain is very subjective and varies from person to person and involves breast size, how much compression is needed to get a clear image, and if your breasts are more sensitive due to where you are in your menstrual cycle. If you feel severe pain or pinching, tell the mammographer.
WHAT WILL THE RESULTS REVEAL?
A mammogram will reveal changes in breast tissue. These changes can be harmless or benign. Most importantly the results can show changes in breast tissue that could indicate early breast cancer. Even with digital mammograms, you will not get your test results right away. This is because the radiologist needs to read the results carefully. You should receive the results of a yearly screening mammogram within 2 to 4 weeks. Diagnostic mammogram results are usually given sooner. Ask the mammographer or your doctor when you can expect your results.
IS THERE ANYTHING I SHOULD DO AFTER MY MAMMOGRAM?
When the mammogram is finished, you can resume your normal activities right away.
DISCLAIMER
This patient education page is for information purposes and is not considered individual patient advice. Because of the changing nature of clinical information and recommendations, please always consult and verify with your physician, pharmacist, or health care provider about specific use or questions. Hermes Health represents that the information provided was formulated with a reasonable standard of care, in conformity with professional standards in the field, and researched with reliable and verified sources.
Colon Cancer Screening
WHAT IS COLON CANCER SCREENING?
Colon screening is an important part of a preventative healthcare plan. The various screening methods all look for early signs of colon cancer in different ways.
WHY GET SCREENED FOR COLON CANCER?
Colon cancer is the third most common cancer in both men and women of all races. Some racial groups are at higher risk than others. The American Cancer Society and The U.S. Preventive Services Task Force recommend people at average risk of colorectal cancer begin screening at around 45 years of age. Screening can be accomplished with either the at-home stool testing kits or via colonoscopy.
HOW OFTEN SHOULD I GET SCREENED?
How often to get screened varies depending on your risk factors and which test you screened with. General recommendations are:
HOW SHOULD I PREPARE FOR THE DIFFERENT TESTS?
There is very little prep for the at-home stool tests other than collecting a sample from your bowel movement.
If you are having a colonoscopy you will have about a 24-hour bowel prep and liquid diet. What specific preparation, diet items, liquids allowed, and bowel evacuation procedure differs by hospital and gastroenterologist who perform the procedure. Detailed instructions will be provided once your appointment is made.
QUESTIONS YOU MAY WANT TO ASK?
HOW ARE THE TESTS PERFORMED?
The at-home tests require obtaining a stool sample from your bowel movement and sending it for testing.
A colonoscopy will be done as an outpatient procedure either at a hospital or a day surgery/procedure center. The test will be performed by a gastroenterologist. It involves visually examining your rectum and colon via a lighted sigmoidoscope (a thin, flexible tube). The scope can also take a sample of tissue or remove polyps if found.
DO THE TESTS HURT?
The at-home stool tests do not cause any discomfort. The colonoscopy is generally not painful because you will be sedated during the procedure. Most complaints of the discomfort of a colonoscopy are related to the 24-hour bowel prep and other pre-procedure preparations done at the hospital.
WHAT WILL THE RESULTS REVEAL?
Hopefully, nothing will be detected. Should the at-home tests detect blood, occult blood, or abnormal DNA, you will be referred and sent for a colonoscopy.
For the colonoscopy, any removed cells or polyps will be sent for testing or biopsy.
The results of all the tests will be reported to your healthcare provider and relayed to you along with any recommended follow-up.
IS THERE ANYTHING I SHOULD DO AFTER MY TEST?
For the at-home stool tests, no further action is required other than following the instructions on how to return the test for diagnostic testing.
For your colonoscopy, you need to have someone accompany you to your procedure so that they can drive you home. You will be groggy from the sedation. Most people are very hungry because of the preparation, but it is suggested to start with light, bland food to avoid nausea and vomiting.
DISCLAIMER
This patient education page is for information purposes and is not considered individual patient advice. Because of the changing nature of clinical information and recommendations, please always consult and verify with your physician, pharmacist, or health care provider about specific use or questions. Hermes Health represents that the information provided was formulated with a reasonable standard of care, in conformity with professional standards in the field, and researched with reliable and verified sources.
Colon screening is an important part of a preventative healthcare plan. The various screening methods all look for early signs of colon cancer in different ways.
- FIT/FOBT: stands for fecal immunochemical test (FIT) fecal occult blood test (FOBT)
- Detects blood in your stool sample
- Can be done at home with no preparation
- Multi-target stool DNA test (such as Cologuard)
- Detects abnormal DNA and blood in your stool sample
- Can be done at home with no preparation
- Colonoscopy
- Visual exam, via a scope, of your colon and rectum
- Performed by a gastroenterologist, at a hospital, as an outpatient procedure
- Requires bowel preparation the day before
- Can remove any suspicious polyps or spots at the time of the exam
WHY GET SCREENED FOR COLON CANCER?
Colon cancer is the third most common cancer in both men and women of all races. Some racial groups are at higher risk than others. The American Cancer Society and The U.S. Preventive Services Task Force recommend people at average risk of colorectal cancer begin screening at around 45 years of age. Screening can be accomplished with either the at-home stool testing kits or via colonoscopy.
HOW OFTEN SHOULD I GET SCREENED?
How often to get screened varies depending on your risk factors and which test you screened with. General recommendations are:
- Stool FIT & FOBT every year
- Multi-target stool DNA test every 3 years
- Colonoscopy every 5-10 years
HOW SHOULD I PREPARE FOR THE DIFFERENT TESTS?
There is very little prep for the at-home stool tests other than collecting a sample from your bowel movement.
If you are having a colonoscopy you will have about a 24-hour bowel prep and liquid diet. What specific preparation, diet items, liquids allowed, and bowel evacuation procedure differs by hospital and gastroenterologist who perform the procedure. Detailed instructions will be provided once your appointment is made.
QUESTIONS YOU MAY WANT TO ASK?
- Which screening test is best for you?
- Always confirm with your healthcare provider if you don’t understand your instructions.
HOW ARE THE TESTS PERFORMED?
The at-home tests require obtaining a stool sample from your bowel movement and sending it for testing.
A colonoscopy will be done as an outpatient procedure either at a hospital or a day surgery/procedure center. The test will be performed by a gastroenterologist. It involves visually examining your rectum and colon via a lighted sigmoidoscope (a thin, flexible tube). The scope can also take a sample of tissue or remove polyps if found.
DO THE TESTS HURT?
The at-home stool tests do not cause any discomfort. The colonoscopy is generally not painful because you will be sedated during the procedure. Most complaints of the discomfort of a colonoscopy are related to the 24-hour bowel prep and other pre-procedure preparations done at the hospital.
WHAT WILL THE RESULTS REVEAL?
Hopefully, nothing will be detected. Should the at-home tests detect blood, occult blood, or abnormal DNA, you will be referred and sent for a colonoscopy.
For the colonoscopy, any removed cells or polyps will be sent for testing or biopsy.
The results of all the tests will be reported to your healthcare provider and relayed to you along with any recommended follow-up.
IS THERE ANYTHING I SHOULD DO AFTER MY TEST?
For the at-home stool tests, no further action is required other than following the instructions on how to return the test for diagnostic testing.
For your colonoscopy, you need to have someone accompany you to your procedure so that they can drive you home. You will be groggy from the sedation. Most people are very hungry because of the preparation, but it is suggested to start with light, bland food to avoid nausea and vomiting.
DISCLAIMER
This patient education page is for information purposes and is not considered individual patient advice. Because of the changing nature of clinical information and recommendations, please always consult and verify with your physician, pharmacist, or health care provider about specific use or questions. Hermes Health represents that the information provided was formulated with a reasonable standard of care, in conformity with professional standards in the field, and researched with reliable and verified sources.
Botox for Migraine Headaches
WHAT ARE BOTOX INJECTIONS FOR MIGRAINES?
Botox has been approved by the FDA for treating migraines. It was approved for the treatment of chronic migraines. Chronic migraines are defined as having a migraine headache 15 or more days per month. Botox is not recommended for less frequent migraines. Botox is the same medicine used in cosmetic procedures, botulinum toxin. Botulinum toxin is a neurotoxin produced by the bacteria that causes botulism. When scientifically processed and then injected into muscles, will cause paralysis that relaxes muscles. The injections are administered at migraine trigger points on your face, head, and back of the neck.
WHY GET BOTOX INJECTIONS?
Many migraine sufferers have reported successful relief from migraines with Botox injections. Some report relief within 1 month of their first treatment. Clinical trials so far have been very promising.
HOW OFTEN DO I GET THE INJECTIONS?
Injection treatments are generally once every 12 weeks. It can take up to six months to see the maximum benefit from Botox. In the meantime, you can continue your regular medications with no risk of drug interaction.
HOW SHOULD I PREPARE FOR A BOTOX INJECTION APPOINTMENT?
The appointment takes roughly 20 minutes. If you are concerned about injection discomfort, you could take an over-the-counter pain reliever 1 hour prior to your appointments.
Avoid face creams, makeup, lotions, perfume, and hair styling products. If you have long hair, wear it up or bring an elastic band or clip to put your hair up.
QUESTIONS YOU MAY WANT TO ASK?
- Are the treatments covered by my insurance?
- Are there any side effects that I should be concerned about?
HOW ARE THE INJECTIONS PERFORMED?
Your healthcare provider will use a very small needle to inject small amounts of Botox into the superficial (surface) muscles in the skin. The injections typically involve multiple injections in several specific areas of the head, face, and neck.
DO THE INJECTIONS HURT?
The injections have been reported to have a minor sting-type feeling. A common side effect of Botox injections is a sore neck. Over-the-counter pain relievers or placing an ice pack on your neck after your appointment reduces discomfort.
WHAT WILL THE RESULTS BE?
Ultimately the results and goal are for you to have a reduction in the number and intensity of your migraines. Some patients have reported relief 2 to 3 weeks after their first appointment.
IS THERE ANYTHING I SHOULD DO AFTER MY INJECTIONS?
Yes - Stay upright for 4 hours. That means keeping your head above heart level. Avoid strenuous activity for the remainder of the day. This is to reduce any risk of swelling and bruising. With all medications, there is always an individual risk of allergic reaction. Notify your healthcare provider if you experience any signs of allergic reaction such as hives, itching, or shortness of breath.
DISCLAIMER
This patient education page is for information purposes and is not considered individual patient advice. Because of the changing nature of clinical information and recommendations, please always consult and verify with your physician, pharmacist, or health care provider about specific use or questions. Hermes Health represents that the information provided was formulated with a reasonable standard of care, in conformity with professional standards in the field, and researched with reliable and verified sources.
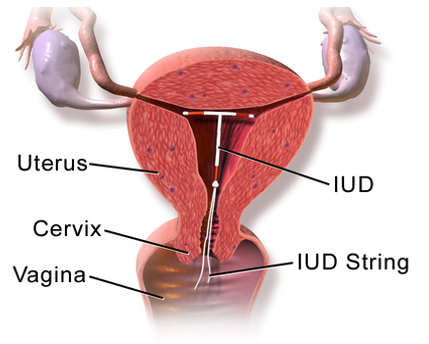
IUD (intrauterine Device)
WHAT IS AN IUD?
An IUD is a medical abbreviation for an Intrauterine Device. An IUD is a plastic or copper, T-shaped device that is inserted into your uterus, to sit near the top. IUDs are a popular form of birth control, providing 99% effectiveness. They can remain implanted for 3-10 years depending on the type. There are two main material types of IUDs available in the United States. One is the copper IUD, Trade name ParaGard, which is non-hormonal. The other two are plastic and release hormonal medication, progestin, Trade names are Mirena, Kyleena, Liletta, and Skyla.
WHAT ARE THE BENEFITS OF AN IUD?
The benefits of an IUD are that it is a highly effective and reversible form of birth control. It requires very minimal upkeep other than periodically checking string placement. An IUD is also one of the best cost-effective forms of contraception for long-term use.
WHAT ARE THE RISKS OF AN IUD?
IUDs are contraindicated, or not recommended, in women with any of the following:
HOW SHOULD I PREPARE FOR THE INSERTION OF MY IUD?
There are several suggested ways that you can prepare for your IUD insertion procedure. Always clarify specific instructions with your healthcare provider. Some common recommendations to ease the procedure discomfort:
QUESTIONS YOU MAY WANT TO ASK?
HOW IS THE IUD INSERTION PERFORMED?
IUD insertion is an outpatient procedure. It is performed by a trained healthcare professional in their office or clinic. The insertion is timed during your menstrual cycle. The timing depends on your healthcare provider and IUD manufacturer recommendations. You will be on a table with your feet in stirrups, just like during your annual pap smear. Your vagina will be held open with a speculum. Before placing the IUD, your provider will wash your cervix and vagina with an antiseptic solution. Then your provider will slide a plastic tube that contains the IUD through your vagina and cervical opening and into your uterus, pushing the IUD into the uterus with the plunger. They will then remove the insertion tube, leaving two small strings that dangle outside your cervix within the vagina.
DOES IUD INSERTION HURT?
There are two parts of the insertion procedure that can cause the most pain or discomfort. The insertion itself can be painful, particularly when your cervix is adjusted to align with your uterus, and then as the insertion tube passes through your cervix, these are generally quick. Once your IUD is placed, the uterus can contract due to irritation, this can lead to cramping.
IS THERE ANYTHING I SHOULD DO AFTER MY IUD IS INSERTED?
If you are having discomfort after the insertion procedure, you may take over-the-counter pain relievers such as acetaminophen (Tylenol) or ibuprofen (Advil). Follow the dosing schedule (don’t take too soon after taking before the insertion procedure to avoid potential overdose). A heating pad can help with any cramping. You can resume your normal activities as soon as you feel able. You may have irregular bleeding, but the bleeding should not be heavy. Many women are unable to feel their IUD strings after the insertion procedure. It is important to notify your doctor if you have heavy bleeding or cramps that are not controlled by over-the-counter pain medications. If you have any concerns, it is important to notify your doctor.
DISCLAIMER
This patient education page is for information purposes and is not considered individual patient advice. Because of the changing nature of clinical information and recommendations, please always consult and verify with your physician, pharmacist, or health care provider about specific use or questions. Hermes Health represents that the information provided was formulated with a reasonable standard of care, in conformity with professional standards in the field, and researched with reliable and verified sources.
An IUD is a medical abbreviation for an Intrauterine Device. An IUD is a plastic or copper, T-shaped device that is inserted into your uterus, to sit near the top. IUDs are a popular form of birth control, providing 99% effectiveness. They can remain implanted for 3-10 years depending on the type. There are two main material types of IUDs available in the United States. One is the copper IUD, Trade name ParaGard, which is non-hormonal. The other two are plastic and release hormonal medication, progestin, Trade names are Mirena, Kyleena, Liletta, and Skyla.
WHAT ARE THE BENEFITS OF AN IUD?
The benefits of an IUD are that it is a highly effective and reversible form of birth control. It requires very minimal upkeep other than periodically checking string placement. An IUD is also one of the best cost-effective forms of contraception for long-term use.
WHAT ARE THE RISKS OF AN IUD?
IUDs are contraindicated, or not recommended, in women with any of the following:
- Pregnant
- Abnormal uterine shape
- Unexplained vaginal bleeding (other than your period)
- Gestational trophoblastic disease
- Pelvic infections, insertion is possible after successful treatment
- Pelvic inflammatory disease
- Cervicitis
- Various other infections that your doctor will discuss with you
- A recent diagnosis of cervical cancer
- A copper allergy, if having ParaGard inserted
- A history of breast or liver cancer, if having levonorgestrel-releasing IUD placed
HOW SHOULD I PREPARE FOR THE INSERTION OF MY IUD?
There are several suggested ways that you can prepare for your IUD insertion procedure. Always clarify specific instructions with your healthcare provider. Some common recommendations to ease the procedure discomfort:
- Take an over-the-counter pain reliever such as acetaminophen (Tylenol) or ibuprofen (Advil). Take about half an hour before your appointment.
- Eat a light meal or a snack before your procedure. Some women have reported dizziness when they stand after the procedure. You can reduce the likelihood of getting dizzy if you have a little food in your system.
- It is also recommended to drink plenty of water the day before your appointment so that you are adequately hydrated.
- Your doctor may want a urine sample or blood test to ensure that you are not pregnant.
- Try to relax and breathe deeply during the procedure.
QUESTIONS YOU MAY WANT TO ASK?
- Specific pre-insertion preparation recommended.
- After insertion instructions.
- Routine hygiene and maintenance instructions for your IUD.
HOW IS THE IUD INSERTION PERFORMED?
IUD insertion is an outpatient procedure. It is performed by a trained healthcare professional in their office or clinic. The insertion is timed during your menstrual cycle. The timing depends on your healthcare provider and IUD manufacturer recommendations. You will be on a table with your feet in stirrups, just like during your annual pap smear. Your vagina will be held open with a speculum. Before placing the IUD, your provider will wash your cervix and vagina with an antiseptic solution. Then your provider will slide a plastic tube that contains the IUD through your vagina and cervical opening and into your uterus, pushing the IUD into the uterus with the plunger. They will then remove the insertion tube, leaving two small strings that dangle outside your cervix within the vagina.
DOES IUD INSERTION HURT?
There are two parts of the insertion procedure that can cause the most pain or discomfort. The insertion itself can be painful, particularly when your cervix is adjusted to align with your uterus, and then as the insertion tube passes through your cervix, these are generally quick. Once your IUD is placed, the uterus can contract due to irritation, this can lead to cramping.
IS THERE ANYTHING I SHOULD DO AFTER MY IUD IS INSERTED?
If you are having discomfort after the insertion procedure, you may take over-the-counter pain relievers such as acetaminophen (Tylenol) or ibuprofen (Advil). Follow the dosing schedule (don’t take too soon after taking before the insertion procedure to avoid potential overdose). A heating pad can help with any cramping. You can resume your normal activities as soon as you feel able. You may have irregular bleeding, but the bleeding should not be heavy. Many women are unable to feel their IUD strings after the insertion procedure. It is important to notify your doctor if you have heavy bleeding or cramps that are not controlled by over-the-counter pain medications. If you have any concerns, it is important to notify your doctor.
DISCLAIMER
This patient education page is for information purposes and is not considered individual patient advice. Because of the changing nature of clinical information and recommendations, please always consult and verify with your physician, pharmacist, or health care provider about specific use or questions. Hermes Health represents that the information provided was formulated with a reasonable standard of care, in conformity with professional standards in the field, and researched with reliable and verified sources.
Depo Shot
WHAT IS A DEPO-PROVERA INJECTION?
The Depo-Provera injection is a shot for contraception. Depo-Provera is the brand name for a drug whose active ingredient is medroxyprogesterone acetate which is derived from progesterone and is available as a generic. Depo-Provera is only used for the prevention of pregnancy. It does not protect you from sexually transmitted diseases. It is given every 3 months as either an intramuscular injection (in the muscle) or as a subcutaneous injection (under the skin).
WHY GET A DEPO-PROVERA INJECTION?
Birth control has many options. The Depo-Provera shot provides these benefits:
- Not having to take a daily birth control pill.
- You have had problems with estrogen-based birth control.
- Reduction in menstrual cramps and discomfort.
- Decrease in menstrual flow and amount.
- You don’t want to interrupt sex for contraception.
- Can decrease the risk of endometrial cancer.
- Is a good option for some health conditions such as anemia or endometriosis.
HOW OFTEN DO I GET A DEPO-PROVERA INJECTION?
The injection is every 3 months. 12-14 weeks depending on which form you receive.
HOW SHOULD I PREPARE FOR MY INJECTION?
There are no recommended pre-injection preparations. There is timing with your periods and when you get your injection. If you get the injection in the first 7 days of your cycle, it works right away. Otherwise, you will need alternate forms of birth control for a month.
QUESTIONS YOU MAY WANT TO ASK?
- Are there any reasons I should not use Depo-Provera as birth control?
- If you have any of the following:
- If you are of think you might be pregnant
- Vaginal bleeding that is not menstrual-related (undiagnosed)
- If you have breast cancer or malignancy
- Liver disease
- Have had adverse reactions to progesterone based birth control
- Certain blood disorders
- If you have any of the following:
- If you have concerns about any potential side effects.
HOW IS THE INJECTION PERFORMED?
The injection comes in 2 different forms. Your healthcare provider may have a single dose (pre-filled) syringe or single-dose vial.
- Depo-Provera vial and pre-filled syringe: Your healthcare provider will inject the shot into a large muscle every 3 months (13 weeks).
- Depo-Provera subcutaneous pre-filled syringe: Your healthcare provider will inject the shot beneath the skin (subcutaneously) every 12 to 14 weeks.
DOES THE INJECTION HURT?
All injections can cause a pinch-like feeling. Most people experience no discomfort. The key is to relax. A muscle, tensed up in apprehension, will feel more discomfort. Some people experience the sensation of the medication going into the muscle, which is described as an odd sensation, but not painful. Some injections cause a sore muscle or red bump at the injection site. All these sensations are normal and brief. An over-the-counter pain reliever can be taken if discomfort occurs after your shot.
ARE THERE ANY SIDE EFFECTS FROM DEPO-PROVERA?
Most hormonal forms of birth control have some side effects. Side effects vary from person to person. What one individual experiences another may not. The common side effects could include:
- Irregular or no periods
- Delayed ovulation
- Weight gain
- Loss of bone mineral density, more common with extended use
- Injection site reactions
- Depression
- Other less frequent side effects could include:
- Headaches, dizziness, and fatigue
IS THERE ANYTHING I SHOULD DO AFTER MY INJECTION?
There are no recommendations for activity or self-care after your injection. If you are having discomfort at the injection site, you may take over-the-counter pain relievers such as acetaminophen (Tylenol) or ibuprofen (Advil). With all injections or medications, there is always an individual risk of allergic reaction. Notify your healthcare provider if you experience any signs of allergic reaction such as hives, itching, or shortness of breath.
DISCLAIMER
This patient education page is for information purposes and is not considered individual patient advice. Because of the changing nature of clinical information and recommendations, please always consult and verify with your physician, pharmacist, or health care provider about specific use or questions. Hermes Health represents that the information provided was formulated with a reasonable standard of care, in conformity with professional standards in the field, and researched with reliable and verified sources.
Trigger Point Injections
WHAT ARE TRIGGER POINT INJECTIONS?
A trigger point injection, sometimes referred to as TPI, is a shot, known as an injection, that is given into muscle tissue at the sight of a knot (tight/taught portion), known as a trigger point. This injection can relieve discomfort and pain in the affected muscle(s). The medication that is injected often contains a local anesthetic or saline and might also include a corticosteroid for inflammation relief. In some cases, no medication is injected, and the trigger point is injected with just the needle, known as dry needling. Injections are performed to provide relief from conditions such as pain from an injury, chronic pain, stress and tension, and muscular disorders. Trigger point injections are often used in combined treatment along with other forms of care, such as muscle relaxants, physical therapy, or massage therapy.
WHY GET A TRIGGER POINT INJECTION?
Pain has a major adverse impact on day-to-day activities. Often hampering plans and limiting mobility. Trigger point injections can provide relief through injections directly into your muscle(s). These injections are aimed at relaxing the tensed up or knotted muscle which provides relief from pain, discomfort, stiffness, and difficulties with range-of-motion or normal movement.
HOW OFTEN SHOULD I GET TRIGGER POINT INJECTIONS?
The frequency of receiving your injections will depend on what you are being treated for and where your trigger points are. How often do the trigger points recur? Your healthcare provider will discuss your plan of care and explain how often your schedule should be. Generally, your treatment results, the condition being treated, and the return of trigger points will determine the frequency of additional treatments.
HOW SHOULD I PREPARE FOR A TRIGGER POINT INJECTION?
There are no pre-injection preparations that are recommended. Let your healthcare provider know if you’ve ever experienced an allergic reaction to a steroid or pain medication or if you have a bleeding disorder.
HOW IS THE INJECTION PERFORMED?
Depending on where you are receiving your injection(s), you will either be lying down or sitting in a comfortable position. The skin over the targeted trigger point(s) is cleaned with an antiseptic solution. Your doctor will insert a needle into the targeted area(s) and inject the prescribed medication or solution. The procedure takes just a few minutes. Your health care provider will perform this at their office.
DOES THE INJECTION HURT?
Injections can cause a pinch-like feeling. Most people experience very minimal discomfort. The key is to relax. Some people experience the sensation of the medication going into the muscle, which is described as an odd sensation, but not painful. Some injections can cause tenderness at the injection site. All these sensations are normal and brief. An over-the-counter pain reliever can be taken if discomfort occurs after your injection.
IS THERE ANYTHING I SHOULD DO AFTER MY INJECTION?
You will likely have relief from muscle pain(s) and you will want to do something you’ve been limited in doing. Don’t overdo it, it’s recommended to relax the treated muscle and only do minor range- of- motions and stretching, not overstretching. Stretching exercises after your injection(s) will be covered by your healthcare provider, based on your condition. Behavior or movement modification is recommended when the trigger points are re-injured due to repetitive tasks. With all injections or medications, there is always an individual risk of allergic reaction. Notify your healthcare provider if you experience any signs of allergic reaction such as hives, itching, or shortness of breath. Notify your healthcare provider if you have any other unusual discomfort, dizziness, bruising, or bleeding at the injection site(s). Having what’s known as a steroid flare is normal, this involves flushing of the face.
DISCLAIMER
This patient education page is for information purposes and is not considered individual patient advice. Because of the changing nature of clinical information and recommendations, please always consult and verify with your physician, pharmacist, or health care provider about specific use or questions. Hermes Health represents that the information provided was formulated with a reasonable standard of care, in conformity with professional standards in the field, and researched with reliable and verified sources.
Joint Injections
WHAT IS A JOINT INJECTION?
A joint injection is a shot that’s given to relieve discomfort and pain in a joint. Joints are categorized into 3 categories: major joints (ie. knees, hips, shoulders), intermediate joints (ie. wrists, ankles, elbows) and small joints (ie. fingers, toes). The medication that is injected is usually a combination of a pain reliever, often lidocaine, and a steroid (for inflammation), usually cortisone. Joint injections are performed to provide relief from conditions such as pain from an injury, simple wear and tear, or an inflammatory disease such as rheumatoid arthritis. For osteoarthritis hyaluronic acid is injected to provide cushioning and lubricating relief.
Sometimes a joint injection is an aspiration, which is the removal of joint fluid. This is usually performed to obtain a sample of your joint fluid to send for laboratory analysis. Getting some extra fluid off an inflamed, swollen joint space does also provide some relief.
WHY GET A JOINT INJECTION?
Joint pain has a major adverse impact on day-to-day activities. Often hampering plans and limiting mobility. Aspiration can provide relief in the mere fact of removing excess fluid and relieving the pressure of swelling. The injection “shot” will provide relief via the medications injected, both towards pain and inflammation. Both aspiration and injection should improve mobility, range of motion, discomfort
HOW OFTEN SHOULD I GET JOINT INJECTIONS?
The frequency of receiving your injections will depend on what you are being treated for. Your healthcare provider will discuss your plan of care and explain how often your schedule should be. Generally, depending on your treatment, it will be as often as monthly, every three months, or every six months.
HOW SHOULD I PREPARE FOR A JOINT INJECTION?
There are no pre-injection or aspiration preparations that are recommended. Let your healthcare provider know if you’ve ever experienced an allergic reaction to a steroid or pain medication. Notify your healthcare provider if you are pregnant, might be pregnant, or are breastfeeding.
QUESTIONS YOU MAY WANT TO ASK?
HOW IS THE INJECTION PERFORMED?
The skin over the targeted joint is cleaned with an antiseptic solution and then injected with a local anesthetic to numb the area. The doctor will insert a needle into the targeted joint and inject a combination of anesthetic and steroids, or hyaluronic acid. If aspiration, the empty syringe will be inserted into the joint space and excess joint fluid will be removed. The procedure takes approximately 10 to 20 minutes. Your health care provider will perform this at their office.
DOES THE INJECTION HURT?
Injections can cause a pinch-like feeling. Most people experience very minimal discomfort. The key is to relax. Some people experience the sensation of the medication going into the joint space, which is described as an odd sensation, but not painful. Some injections cause a sore tendon near the injection or a red mark at the injection site. All these sensations are normal and brief. An over-the-counter pain reliever can be taken if discomfort occurs after your injection.
IS THERE ANYTHING I SHOULD DO AFTER MY INJECTION?
There are no recommendations for activity or self-care after your injection or aspiration. You will likely have such relief that you will want to do something you’ve been limited in doing. Don’t overdo it. With all injections or medications, there is always an individual risk of allergic reaction. Notify your healthcare provider if you experience any signs of allergic reaction such as hives, itching, or shortness of breath. Notify your healthcare provider if you have any other unusual discomfort. Having what’s known as a steroid flare is normal, this involves flushing of the face.
A joint injection is a shot that’s given to relieve discomfort and pain in a joint. Joints are categorized into 3 categories: major joints (ie. knees, hips, shoulders), intermediate joints (ie. wrists, ankles, elbows) and small joints (ie. fingers, toes). The medication that is injected is usually a combination of a pain reliever, often lidocaine, and a steroid (for inflammation), usually cortisone. Joint injections are performed to provide relief from conditions such as pain from an injury, simple wear and tear, or an inflammatory disease such as rheumatoid arthritis. For osteoarthritis hyaluronic acid is injected to provide cushioning and lubricating relief.
Sometimes a joint injection is an aspiration, which is the removal of joint fluid. This is usually performed to obtain a sample of your joint fluid to send for laboratory analysis. Getting some extra fluid off an inflamed, swollen joint space does also provide some relief.
WHY GET A JOINT INJECTION?
Joint pain has a major adverse impact on day-to-day activities. Often hampering plans and limiting mobility. Aspiration can provide relief in the mere fact of removing excess fluid and relieving the pressure of swelling. The injection “shot” will provide relief via the medications injected, both towards pain and inflammation. Both aspiration and injection should improve mobility, range of motion, discomfort
HOW OFTEN SHOULD I GET JOINT INJECTIONS?
The frequency of receiving your injections will depend on what you are being treated for. Your healthcare provider will discuss your plan of care and explain how often your schedule should be. Generally, depending on your treatment, it will be as often as monthly, every three months, or every six months.
HOW SHOULD I PREPARE FOR A JOINT INJECTION?
There are no pre-injection or aspiration preparations that are recommended. Let your healthcare provider know if you’ve ever experienced an allergic reaction to a steroid or pain medication. Notify your healthcare provider if you are pregnant, might be pregnant, or are breastfeeding.
QUESTIONS YOU MAY WANT TO ASK?
- What will be the frequency of my injections?
- Specific side effects for the medications being injected?
- What brand am I being injected
HOW IS THE INJECTION PERFORMED?
The skin over the targeted joint is cleaned with an antiseptic solution and then injected with a local anesthetic to numb the area. The doctor will insert a needle into the targeted joint and inject a combination of anesthetic and steroids, or hyaluronic acid. If aspiration, the empty syringe will be inserted into the joint space and excess joint fluid will be removed. The procedure takes approximately 10 to 20 minutes. Your health care provider will perform this at their office.
DOES THE INJECTION HURT?
Injections can cause a pinch-like feeling. Most people experience very minimal discomfort. The key is to relax. Some people experience the sensation of the medication going into the joint space, which is described as an odd sensation, but not painful. Some injections cause a sore tendon near the injection or a red mark at the injection site. All these sensations are normal and brief. An over-the-counter pain reliever can be taken if discomfort occurs after your injection.
IS THERE ANYTHING I SHOULD DO AFTER MY INJECTION?
There are no recommendations for activity or self-care after your injection or aspiration. You will likely have such relief that you will want to do something you’ve been limited in doing. Don’t overdo it. With all injections or medications, there is always an individual risk of allergic reaction. Notify your healthcare provider if you experience any signs of allergic reaction such as hives, itching, or shortness of breath. Notify your healthcare provider if you have any other unusual discomfort. Having what’s known as a steroid flare is normal, this involves flushing of the face.
DISCLAIMER
This patient education page is for information purposes and is not considered individual patient advice. Because of the changing nature of clinical information and recommendations, please always consult and verify with your physician, pharmacist, or health care provider about specific use or questions. Hermes Health represents that the information provided was formulated with a reasonable standard of care, in conformity with professional standards in the field, and researched with reliable and verified sources.
This patient education page is for information purposes and is not considered individual patient advice. Because of the changing nature of clinical information and recommendations, please always consult and verify with your physician, pharmacist, or health care provider about specific use or questions. Hermes Health represents that the information provided was formulated with a reasonable standard of care, in conformity with professional standards in the field, and researched with reliable and verified sources.
B12 Injections
WHAT IS A B12 INJECTION?
A B12 injection is a shot that’s given to correct low levels of vitamin B12. Cyanocobalamin is the name for this man-made vitamin B12 form. Vitamin B12 is important for the growth of healthy blood cells, nerve cells, and proteins in the body. It also aids in the metabolism of fats and carbohydrates. People normally absorb the required amount of B12 through their diet in the foods they consume. Vitamin B12 is present naturally in foods of animal origin, such as meats, eggs, and dairy products. It is also added to some fortified foods, such as cereals.
WHY GET A B12 INJECTION?
B12 is an important vitamin for the human body. We primarily get natural vitamin B12 through the foods we eat. B12 is absorbed naturally in our intestines. Some people can’t or don’t absorb enough vitamin B12 to maintain healthy or adequate levels. That deficiency is corrected through B12 injections. Certain conditions and diets affect B12 levels in the body, such as:
HOW OFTEN SHOULD I GET A B12 INJECTION?
The frequency of receiving your injections will depend on what you are being treated for. With pernicious anemia, you may start with daily injections, and then gradually begin extending the time between injections. Some individuals receive monthly injections. Your healthcare provider will discuss your plan of care and explain how often your schedule should be.
HOW SHOULD I PREPARE FOR A B12 INJECTION?
There are no pre-injection preparations that are recommended. Your healthcare provider may draw your blood for laboratory testing to establish a baseline B12 level to monitor your levels as treatment progresses. Let your healthcare provider know if you’ve ever experienced an allergic reaction to supplements or vitamins. Notify your healthcare provider if you are pregnant, might be pregnant, or are breastfeeding.
QUESTIONS YOU MAY WANT TO ASK?
HOW IS THE INJECTION PERFORMED?
Vitamin B12 (Cyanocobalamin) comes as a liquid, known as a solution, it will be injected into a muscle (intramuscular) or just under the skin (subcutaneous). Your health care provider will give this injection at their office.
DOES THE INJECTION HURT?
Injections can cause a pinch-like feeling. Most people experience no discomfort. The key is to relax. A muscle, tensed up in apprehension, will feel more discomfort. Some people experience the sensation of the medication going into the muscle, which is described as an odd sensation, but not painful. Some injections cause a sore muscle or red bump at the injection site. All these sensations are normal and brief. An over-the-counter pain reliever can be taken if discomfort occurs after your injection.
IS THERE ANYTHING I SHOULD DO AFTER MY INJECTION?
There are no recommendations for activity or self-care after your injection. Your healthcare provider will perform follow-up labs to monitor your B12 levels. If after your injection, you are having discomfort at the injection site, you may take over-the-counter pain relievers such as acetaminophen (Tylenol) or ibuprofen (Advil). With all injections or medications, there is always an individual risk of allergic reaction. Notify your healthcare provider if you experience any signs of allergic reaction such as hives, itching, or shortness of breath.
DISCLAIMER
This patient education page is for information purposes and is not considered individual patient advice. Because of the changing nature of clinical information and recommendations, please always consult and verify with your physician, pharmacist, or health care provider about specific use or questions. Hermes Health represents that the information provided was formulated with a reasonable standard of care, in conformity with professional standards in the field, and researched with reliable and verified sources.
A B12 injection is a shot that’s given to correct low levels of vitamin B12. Cyanocobalamin is the name for this man-made vitamin B12 form. Vitamin B12 is important for the growth of healthy blood cells, nerve cells, and proteins in the body. It also aids in the metabolism of fats and carbohydrates. People normally absorb the required amount of B12 through their diet in the foods they consume. Vitamin B12 is present naturally in foods of animal origin, such as meats, eggs, and dairy products. It is also added to some fortified foods, such as cereals.
WHY GET A B12 INJECTION?
B12 is an important vitamin for the human body. We primarily get natural vitamin B12 through the foods we eat. B12 is absorbed naturally in our intestines. Some people can’t or don’t absorb enough vitamin B12 to maintain healthy or adequate levels. That deficiency is corrected through B12 injections. Certain conditions and diets affect B12 levels in the body, such as:
- Pernicious anemia.
- Having had surgery on the stomach or intestines.
- Inherited conditions, diseases, infections, or medications that decrease the amount of vitamin B12 absorbed through the intestines from food.
- A strict vegan diet that does not allow any animal products.
HOW OFTEN SHOULD I GET A B12 INJECTION?
The frequency of receiving your injections will depend on what you are being treated for. With pernicious anemia, you may start with daily injections, and then gradually begin extending the time between injections. Some individuals receive monthly injections. Your healthcare provider will discuss your plan of care and explain how often your schedule should be.
HOW SHOULD I PREPARE FOR A B12 INJECTION?
There are no pre-injection preparations that are recommended. Your healthcare provider may draw your blood for laboratory testing to establish a baseline B12 level to monitor your levels as treatment progresses. Let your healthcare provider know if you’ve ever experienced an allergic reaction to supplements or vitamins. Notify your healthcare provider if you are pregnant, might be pregnant, or are breastfeeding.
QUESTIONS YOU MAY WANT TO ASK?
- What will be the frequency of my injections?
- What are the common side effects?
- Diarrhea
- A feeling like your body is swollen
- Will I be able to change to a different form of B12 supplement, such as oral or nasal?
HOW IS THE INJECTION PERFORMED?
Vitamin B12 (Cyanocobalamin) comes as a liquid, known as a solution, it will be injected into a muscle (intramuscular) or just under the skin (subcutaneous). Your health care provider will give this injection at their office.
DOES THE INJECTION HURT?
Injections can cause a pinch-like feeling. Most people experience no discomfort. The key is to relax. A muscle, tensed up in apprehension, will feel more discomfort. Some people experience the sensation of the medication going into the muscle, which is described as an odd sensation, but not painful. Some injections cause a sore muscle or red bump at the injection site. All these sensations are normal and brief. An over-the-counter pain reliever can be taken if discomfort occurs after your injection.
IS THERE ANYTHING I SHOULD DO AFTER MY INJECTION?
There are no recommendations for activity or self-care after your injection. Your healthcare provider will perform follow-up labs to monitor your B12 levels. If after your injection, you are having discomfort at the injection site, you may take over-the-counter pain relievers such as acetaminophen (Tylenol) or ibuprofen (Advil). With all injections or medications, there is always an individual risk of allergic reaction. Notify your healthcare provider if you experience any signs of allergic reaction such as hives, itching, or shortness of breath.
DISCLAIMER
This patient education page is for information purposes and is not considered individual patient advice. Because of the changing nature of clinical information and recommendations, please always consult and verify with your physician, pharmacist, or health care provider about specific use or questions. Hermes Health represents that the information provided was formulated with a reasonable standard of care, in conformity with professional standards in the field, and researched with reliable and verified sources.
Vaccines
WHAT ARE VACCINES?
Vaccines or vaccinations also referred to as immunizations and inoculations, are a form of preventative treatment (by vaccination) to make individuals immune to diseases or other toxic agents. This immunity is obtained by the administration of an immune-producing substance, a vaccination.
WHY GET VACCINES?
Vaccines provide protection to individuals from serious diseases. Being vaccinated is an extremely important part of a healthy life and a preventative healthcare plan. As part of the general population, being vaccinated helps the community by stopping the spread of dangerous and deadly diseases and viruses to persons who are unable to get vaccinated or are at risk for serious complications if infected. The guideline recommendations are put in place by various medical organizations, federal and community health department panels, and boards consisting of healthcare professionals, scientists, and experts in infectious diseases.
WHEN SHOULD I GET VACCINATED?
Vaccine recommendations are scheduled as age-based guidelines. If you are behind or missing recommended vaccinations, there are guidelines for when to get your make-up/catch-up vaccines.
- Vaccinations are mandatory to enter school, participate in sports, travel to certain countries, and join the military.
- Some vaccines received as childhood vaccinations have a recommendation for an adult booster.
- Some vaccines are recommended yearly, such as influenza (flu) and pneumococcal (pneumonia).
- There are vaccines that are recommended while pregnant such as pertussis and influenza.
- Sometimes important vaccines are developed for emergency purposes, such as COVID-19.
VACCINATIONS AVAILABLE AT HERMES HEALTH
- Many of the recommended vaccines come as combination vaccines. This conveniently provides fewer injections.
- CHILDHOOD vaccinations recommended for infants through eighteen years of age.
- Hepatitis B
- A very serious liver disease caused by a virus
- Comes as a scheduled dose, between 2 to 4 doses depending on the manufacturer
- Rotavirus
- A highly contagious gastrointestinal (stomach/bowel) disease
- Provided as a 3-dose schedule
- DTaP vaccine
- Diphtheria
- A serious bacterial infection that affects breathing and the skin
- Tetanus
- A bacterial infection that causes painful muscle contractions or muscles locking up
- Acellular pertussis (pertussis)
- Known as whooping cough which is very serious in infants
- Diphtheria
- Haemophilus influenzae type b
- Can cause severe infections of both the lining of the brain and spinal cord (meningitis) and the bloodstream
- Pneumococcal conjugate
- Pneumococcal infections can range from ear and sinus infections to pneumonia and bloodstream infections
- Inactivated poliovirus
- A disabling and life-threatening disease that can cause paralysis
- Yearly Influenza
- The flu is a yearly respiratory infection (breathing/lungs) that is highly contagious
- Measles, mumps, rubella (MMR)
- Measles: a highly contagious virus that can lead to serious complications. It affects the respiratory system
- Mumps: a contagious disease caused by a virus. Complications include swelling of glands and organs
- Rubella: a contagious disease caused by a virus. Most dangerous to pregnant women if infected
- Varicella
- Known commonly as chickenpox
- Very contagious
- Can be serious and life-threatening, especially in babies, children, and pregnant women
- Hepatitis A
- Is a serious liver disease caused by a virus
- Meningococcal (B and ACWY)
- Often severe, can be deadly
- Can cause infections of the lining of the brain and spinal cord (meningitis) and bloodstream
- Human papillomavirus (HPV)
- HPV is a common virus that can lead to certain types of cancer later in life
- Is given as 3 dose schedule
- Hepatitis B
- ADULT vaccinations recommended from age nineteen years and older
- Yearly Influenza (flu)
- New vaccines formulated every year based on the prior year’s flu strains
- Vaccination prevents serious forms of illness.
- Pregnant women are more likely to have a serious illness with flu.
- Tdap or TD
- Tetanus
- Reduced diphtheria
- Pertussis
- Zoster recombinant
- Herpes zoster, known as shingles, is caused by the reactivation of the varicella-zoster virus (chickenpox)
- Pneumococcal
- Yearly booster
- Hepatitis A & B
- Adult booster or catch-up
- Meningococcal B & ACWY
- Adult booster or catch-up
- Yearly Influenza (flu)
HOW SHOULD I PREPARE FOR A VACCINE?
There are no pre-vaccination preparations that are recommended.
QUESTIONS YOU MAY WANT TO ASK?
- If you are apprehensive about vaccines, talk to your healthcare provider.
- Are there any side effects to be concerned about?
- What are the typical adverse reactions?
HOW ARE VACCINES GIVEN?
Most all vaccinations are given via an intramuscular injection, some can be given via other delivery methods. For intramuscular, a small thin needle with an attached syringe injects the vaccine into a large muscle (upper arm, thigh, or buttocks).
DO VACCINES HURT?
Vaccine injections can cause a pinch-like feeling. Most people experience no discomfort. The key is to relax. A muscle, tensed up in apprehension, will feel more discomfort. Some people experience the sensation of the vaccine going into the muscle, which is described as an odd sensation, but not painful. Some vaccinations cause a sore muscle or red bump at the injection site. All these sensations are normal and brief. An over-the-counter pain reliever can be taken if discomfort occurs after your vaccine.
IS THERE ANYTHING I SHOULD DO AFTER MY VACCINATION?
There are no recommendations for activity or self-care after your vaccine(s). If you are having discomfort at the injection site, you may take over-the-counter pain relievers such as acetaminophen (Tylenol) or ibuprofen (Advil). With all vaccines or medications, there is always an individual risk of allergic reaction. Notify your healthcare provider if you experience any signs of allergic reaction such as hives, itching, or shortness of breath.
DISCLAIMER
This patient education page is for information purposes and is not considered individual patient advice. Because of the changing nature of clinical information and recommendations, please always consult and verify with your physician, pharmacist, or health care provider about specific use or questions. Hermes Health represents that the information provided was formulated with a reasonable standard of care, in conformity with professional standards in the field, and researched with reliable and verified sources.
Skin Tag Removal
WHAT IS SKIN TAG REMOVAL?
Skin tags, called acrochordons are common. The likelihood of developing them increases as we age, so there is a good chance you will develop at least one in your lifetime. Skin tags usually grow in areas where there are skin folds that produce friction, such as the underarms, neck, eyelids, and groin. Even though skin tags aren’t aesthetically pleasing, or unsightly, they are almost always noncancerous and shouldn’t be cause for concern. Skin tag removal from an experienced healthcare provider lowers the risk of complications and minimizes scarring. It is unknown what causes skin tags, but fortunately, they do not pose other health concerns.
WHY GET SKIN TAGS REMOVED?
If the appearance of your skin tag(s) bothers you or they rub against clothing, skin, or jewelry, you can have them removed.Having skin tags removed by a healthcare professional is the best treatment for removal. There are many over-the-counter skin tag removal products, but at-home treatments are not safe. Most are not regulated, or FDA approved, they also come with a higher risk of complications, which include:
- Scars
- Excessive bleeding
- Infection
- Incomplete skin tag removal, which leads to re-occurrence
- Improper application or use
- Damage to healthy nearby skin
- Use on a growth that is not a skin tag (mole or cancerous legion)
HOW SHOULD I PREPARE FOR SKIN TAG REMOVAL?
There are no pre-procedure preparations that are recommended. Depending upon the area(s) where your skin tag is located, avoid the use of:
- Lotions or powders
- Deodorant
- Jewelry
QUESTIONS YOU MAY WANT TO ASK?
- What are the chances of re-occurrence?
- Will this be biopsied
HOW IS THE PROCEDURE PERFORMED?
There are several methods for skin tag removal. Treatment usually takes place during an in-office visit > The procedure involves:
- A sharp instrument such as a scalpel or surgical scissors to cut it off
- Liquid nitrogen to freeze it
- Heat, known as electrocautery, in order to burn it off or to stop bleeding
DOES THE PROCEDURE HURT?
Skin tag removal procedures can cause discomfort. Usually, you will receive a local numbing medication at the site, such as a spray, topical gel, cream, or injection. This injected medication will numb the area to help alleviate discomfort.
IS THERE ANYTHING I SHOULD DO AFTER REMOVAL?
The treatment area will form a small scab in the next few days following the procedure. Once the scab falls off, you may notice a slight imperfection in the skin. This imperfection will hardly be noticeable to others. Watch for signs of infection, such as redness in the area. As the area heals, you may experience itching which is completely normal.
DISCLAIMER
This patient education page is for information purposes and is not considered individual patient advice. Because of the changing nature of clinical information and recommendations, please always consult and verify with your physician, pharmacist, or health care provider about specific use or questions. Hermes Health represents that the information provided was formulated with a reasonable standard of care, in conformity with professional standards in the field, and researched with reliable and verified sources.